Alcohol Addiction Intervention: How to Stage an Intervention and Help a Loved One Accept Treatment
Key Topics in Alcohol Rehab
When drinking shifts from “concerning” to dangerous, families often try to talk it out, argue it out, or wait it out. None of that is a plan. This guide is built to help a loved one move from denial and delay to a clear next step, while protecting safety, dignity, and privacy.
If you believe your loved one is in immediate danger, call 911 or go to the nearest emergency department. This page is not an emergency service.
-
AI OVERVIEW - ALCOHOL DETOX PROCESS
What is an Alcohol Intervention?
This is a structured, time-limited conversation where friends and family members present clear observations, set boundaries, and offer a specific path to care. It is designed to help someone with an addiction recognize the problem and accept treatment, not to shame them into compliance.
Many people use the term alcoholism casually. Clinically, the focus is on risk, functioning, and alcohol use disorder, not labels.


What “intervention involves” in real life
A “real” approach is calm, planned, and focused on one outcome: a next step today. It usually includes:
- Specific examples of the loved one’s behavior and its impact
- One unified message from the people closest to them
- Boundaries that will be enforced
- A ready-to-go treatment plan and logistics (so there is no scrambling)
Brief intervention vs formal interventionBrief intervention vs formal intervention
A brief intervention is usually a short, clinician-led conversation in a medical setting that highlights risk and recommends a next step. A formal approach is a planned family process built to create accountability and immediate follow-through.

When It’s Time to Intervene for a Loved One
Waiting for “rock bottom” is a myth that costs time, health, and relationships. Addiction may show up as secrecy, volatility, missed obligations, or escalating risk. If you are trying to help someone and the pattern keeps repeating, you likely need a more structured plan.

Signs a loved one may be struggling with alcohol misuse
Your loved one may show a cluster of changes, not one dramatic event. Common signs include:
- Drinking earlier, drinking alone, or hiding it
- Mood swings, irritability, anxiety, or withdrawal from others
- Risky decisions, conflicts at work, or repeated broken promises
- Changes in sleep, appetite, or overall stability
- Increasing tolerance or obvious effects of alcohol use
If you are seeing escalating conflict around drinking habits, the situation is already affecting daily functioning.
Quick Safety Screen Before You Stage an Intervention
Before you do anything, rule out medical and safety risks. If the situation is volatile, the safest move is not a family meeting. It is professional help.
When alcohol use disorder withdrawal is a medical emergency
Alcohol withdrawal can be life-threatening. Seek urgent medical care if there are:
Seizures, severe confusion, hallucinations, or uncontrolled shaking
Chest pain, trouble breathing, fainting, or severe dehydration
High fever, severe agitation, or signs of delirium
If any of these are present, do not attempt a home-based plan.
When to seek professional help immediately
Seek help now if there is:
Threats of self-harm or harm to others
Violence, stalking, weapons, or intimidation
An unsafe home environment for children or vulnerable adults
A pattern of binge drinking with blackout episodes
Evidence-Based Intervention Models
There is no single “best treatment” conversation style. The right approach depends on risk level, family dynamics, and whether the person struggling with addiction is likely to engage voluntarily.
This approach is structured and direct. It uses prepared statements and clear consequences. It can be effective when denial is strong and the family can follow through consistently.
This approach is invitational and stepwise. The person is invited into the process early, with escalation only if they decline. It can reduce defensiveness while still creating urgency.
This approach is skills-based coaching for the family. It focuses on communication, reinforcement of healthy behavior, and reducing reinforcement of harmful behavior. It is often used when a loved one refuses initially.
Intervention Models at a Glance
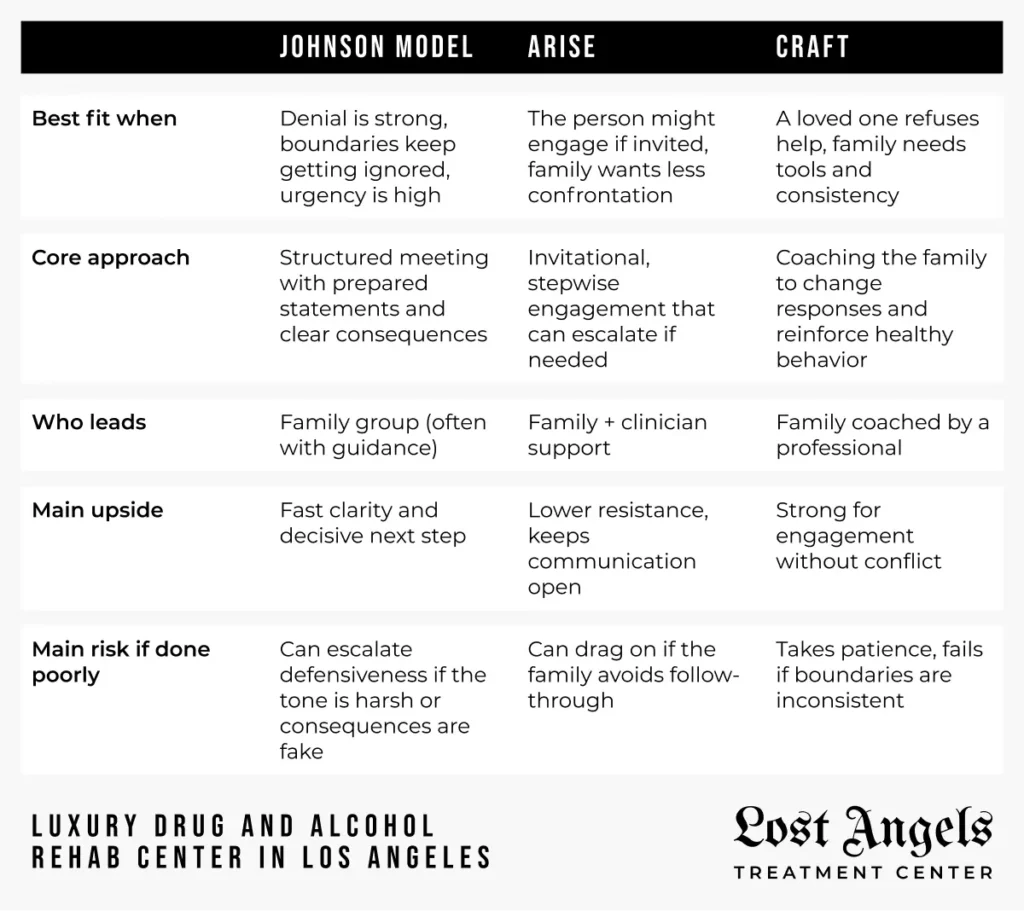
Which model fits a person struggling with addiction?
Choose based on reality, not wishful thinking:
- High conflict or repeated broken agreements: more structure
- Some willingness to talk: invitational approaches
- Safety concerns: prioritize clinical oversight and a rapid referral


Creating a Plan Before You Hold the Intervention
This is where most families fail. They talk first and plan later. Flip it.
Build a plan that covers:
- Who should be present and who should not
- What each person will say, using specific examples without insults
- Boundaries and consequences you can actually enforce
- Treatment options and one clear treatment choice with a confirmed pathway to admission
- Transportation, time off work, and phone expectations
Aim for language that is firm but not cruel, so your loved one doesn’t feel cornered. Be specific about what your loved one needs to change, and what you will do if nothing changes. Your job is to give your loved one a clear choice and a clear next step.
How to Stage an Intervention Step by Step
This is not about perfect wording. It is about preparation, unity, and immediate follow-through.
Stage 1: Prepare the message and roles
Each participant writes a short statement:
- What they have observed (facts)
- How it has affected them (impact)
- The boundary they will keep (action)
- The offer to seek treatment (next step)
Stage 2: Rehearse and set the rules
Rehearse once. Keep it brief. Decide who leads, who reads first, and who stays silent. Set rules: no arguing, no diagnosing, no bargaining.
Stage 3: Hold the intervention and make the ask to accept help
Keep the ask simple: accept help today. Offer a specific treatment program, not a vague promise to “do better.” If someone is addicted to alcohol, ambiguity becomes an escape hatch.
Stage 4: Immediate referral and handoff to a treatment provider
Have the next step ready: a confirmed assessment and intake process with a treatment provider. This is the referral moment. Delay is where momentum dies.
Working With an Interventionist or Intervention Specialist
When the situation is complex, emotionally volatile, or high risk, seeking professional help can protect everyone involved and prevent the meeting from turning into a fight.


What an intervention professional actually does
A qualified specialist can:
- Assess risk and recommend the safest format
- Coach the family on messaging and boundaries
- Coordinate treatment facilities and timing
- Keep the process controlled when emotions spike
When intervention services are worth it
Consider outside support when:
- There is a history of threats, violence, or severe instability
- Multiple substances are involved (alcohol or drug)
- The family is divided or inconsistent
- Prior attempts have failed and trust is low

What Happens After the Intervention
Your job is not to force insight. Your job is follow-through and consistency, even if the first attempt does not go to plan.
Move immediately. Confirm insurance verification, finalize travel, and begin the intake process.
A licensed clinician will complete a comprehensive initial assessment in order to create a treatment approach recommended by the clinical and medical team.
Treatment may start with detox, then step into a structured program. You will be assigned an individual therapist as well.
If a loved one refuses, you still act. Enforce the boundaries you stated. Reduce enabling. Use support groups for yourself. Keep your message consistent and keep the door open to get treatment.
Do not renegotiate. Return to the plan. Repeat the same offer and the same boundary. Consistency is what keeps this from turning into empty threats.
Treatment Choices After a Successful Intervention
This section stays high level on purpose. Your goal is not to debate particulars. Your goal is to match risk to a level of care, then move quickly into addiction treatment.

Detox, inpatient, or outpatient treatment: what type of treatment fits?
In general:
- Detox: medical stabilization when withdrawal risk is present
- Inpatient: structured care when risk is higher or the home environment is unstable
- Outpatient treatment: structured sessions when stability and support are strong
The best treatment is the one that matches risk and is realistic to start immediately. A qualified addiction professional can help match the level of care to risk.
Alcohol or drug concerns: substance use disorders and drug addiction intervention
If the situation involves an alcoholic or drug addict, plan for higher complexity and tighter boundaries. Mixed use often requires a more conservative level of care and clearer monitoring across multiple substances.
Mental health conditions and dual diagnosis in the recovery journey
Anxiety, depression, trauma, and other mental health conditions can drive relapse if untreated. Dual diagnosis care addresses both the addiction and the mental health piece as one integrated plan, which allows your loved one to stabilize and engage in care.
Insurance and Logistics Families Get Wrong
Families often delay because the practical details feel overwhelming. Do not let logistics become an excuse to avoid the next step.
Insurance verification and what treatment may require
Insurance verification may require basic policy details and a clinical assessment. Ask direct questions about covered levels of care, authorizations, and what documentation is needed for admission to treatment centers.


Supporting Long-Term Recovery Without Enabling
Long-term recovery is built on structure and accountability, not repeated rescue missions. Agree on boundaries, follow them, and keep support consistent.
What helps:
- Family education and coaching
- Support groups and 12-step communities when appropriate
- A plan for triggers, relapse risk, and communication
- Ongoing coordination with clinical and admissions teams
If you want to help your loved one, protect your own limits as seriously as you protect their dignity. That is how families stay steady over time.
Ready to Take the Next Step With Lost Angels
If you are trying to help a loved one move from repeated promises to real change, the most important moment is the handoff. Lost Angels Treatment Center provides a discreet, clinically led path into care in Los Angeles, with a structured intake process designed to reduce delays and protect privacy.
Why families choose Lost Angels
Licensed in California: License/registration number 191512AP
Accredited, quality-focused care: Joint Commission accredited
Full continuum: detox, residential, and outpatient options when clinically appropriate
Dual diagnosis capability: support for addiction alongside mental health conditions
Luxury-level privacy and comfort with a serious clinical standard
Psychology Today Profile: Verified listing.
BBB: Business profile
When you are ready, our team can guide you through a confidential assessment and a clear treatment plan, so you are not guessing what level of care is safest.
References
- 1. NIAAA — Alcohol Use Disorder: From Risk to Diagnosis to Recovery
- 2. CDC — Alcohol Use and Your Health
- 3. NCBI Bookshelf (NIH) — Community Reinforcement and Family Training (CRAFT)
- 4. NIAAA — Conduct a Brief Intervention: Build Motivation and a Plan for Change
- 5. MedlinePlus (NIH) — Alcohol withdrawal
Alcohol Intervention FAQs
What is an alcohol intervention?
It is a structured conversation with a clear purpose: align the family, present facts, set boundaries, and offer an immediate next step into care. It should be planned, calm, and focused on safety.
How do you stage an intervention for a loved one?
Plan first. Write short impact statements. Agree on boundaries you will enforce. Line up treatment options and logistics in advance. Then hold the meeting at a calm time with one clear next step.
If safety is unclear, pause and seek help from an experienced professional.
What should you avoid saying so your loved one doesn’t feel judged?
Avoid labels, insults, and ultimatums you cannot enforce. Do not argue about “how much” they drank. Do not debate memories from a blackout. Do not stack accusations. Keep the tone calm and the message consistent.
Should we hire an interventionist or intervention specialist?
Consider it when emotions run high, the family is divided, or there is any safety risk. The right professional protects structure, reduces escalation, and increases follow-through.
Ask whether they coordinate with an addiction specialist or other clinical partners, and whether they can connect you to appropriate levels of care.
Do these meetings work, and what makes an effective intervention?
They work best when the plan is unified and consequences are real. What makes it effective is not pressure. It is clarity, consistency, and immediate access to care, with boundaries the family will actually keep.
What if my loved one refuses to accept help or accept treatment?
Do not chase, bargain, or threaten. Follow through on your stated boundary. Reduce enabling. Get support for yourself. Keep one consistent offer open: a clear path to care when they are ready to seek help.
What happens after they agree to seek treatment?
Move quickly. Confirm logistics, confirm insurance, and schedule intake. If detox is needed, arrange it first. Then transition into the appropriate treatment program with a clear plan for aftercare and ongoing support.
Is an intervention for alcohol covered by insurance?
Coverage varies. Some services are billed under clinical assessment or counseling, while others are private-pay. Ask for a written explanation of costs, what is covered, and what documentation is required.
When is alcohol withdrawal a medical emergency?
If there are seizures, hallucinations, severe confusion, chest pain, trouble breathing, fainting, or signs of delirium, treat it as an emergency. Call 911 or go to the nearest emergency department.